Donación de sangre
Un donante de sangre aporta aproximadamente 500 ml de sangre total, la cual se colecta directamente en un sistema estéril de bolsas. Posteriormente, la unidad es sometida a centrifugación, permitiendo la separación de los componentes celulares del plasma sanguíneo. El proceso produce una bolsa de eritrocitos y otra de plasma recuperado. En algunos bancos de sangre, también se obtiene la fracción rica en plaquetas, es decir, la capa leucoplaquetaria (buffy coat).
Los eritrocitos son insumos fundamentales en el ámbito hospitalario, especialmente para procedimientos quirúrgicos y atención de pacientes en estado crítico.
Asimismo, ciertos tipos específicos de componentes sanguíneos son necesarios para la industria de diagnóstico in vitro.
¿Qué es sangre?
La sangre es un fluido corporal que entrega sustancias esenciales, como nutrientes y oxígeno, a las células. La sangre está compuesta por células sanguíneas suspendidas en el plasma.
Las células sanguíneas son principalmente los eritrocitos (glóbulos rojos), los leucocitos (glóbulos blancos) y las plaquetas (trombocitos). Las células más abundantes son los eritrocitos. El cuerpo humano contiene, en promedio, aproximadamente 5 litros de sangre.
Toda transfusión debe someterse a una prueba de compatibilidad cruzada (crossmatch) para verificar que la sangre del receptor y la unidad de eritrocitos seleccionada sean completamente compatibles.

Las empresas de diagnóstico fabrican kits de prueba especializados para este tipo de análisis.
Esto significa que una donación de sangre destinada a fines diagnósticos salva vidas tanto como una donación de sangre para transfusión humana.
Actualmente no existe un sustituto completo para la sangre, pero sí existen posibilidades para mitigar la pérdida sanguínea en cirugías programadas.
Desde hace más de una década, los sistemas transfusionales a nivel mundial trabajan en el denominado Patient Blood Management (PBM), o gestión del paciente basada en la conservación de la sangre, con el fin de minimizar la transfusión de eritrocitos.
Recupera tu plasma - los pacientes lo necesitan.
Cada donación de sangre puede separarse en concentrado de eritrocitos y plasma. Una pequeña parte de este plasma se utiliza para transfusiones. Sin embargo, la mayor parte se desecha. El 50% de nuestra sangre es plasma. Es la parte líquida. Una donación de 500 ml contiene hasta 300 ml de plasma sanguíneo.
Muchos países alrededor del mundo siguen desechando este plasma en lugar de recuperarlo para fraccionamiento. Pacientes en todo el mundo padecen enfermedades graves y dependen del plasma sanguíneo como materia prima.
La inmunoglobulina, la albúmina humana, los factores de coagulación y muchos otros medicamentos se obtienen del plasma sanguíneo.

Recuperemos el plasma sanguíneo y utilicémoslo para el bien de los pacientes.
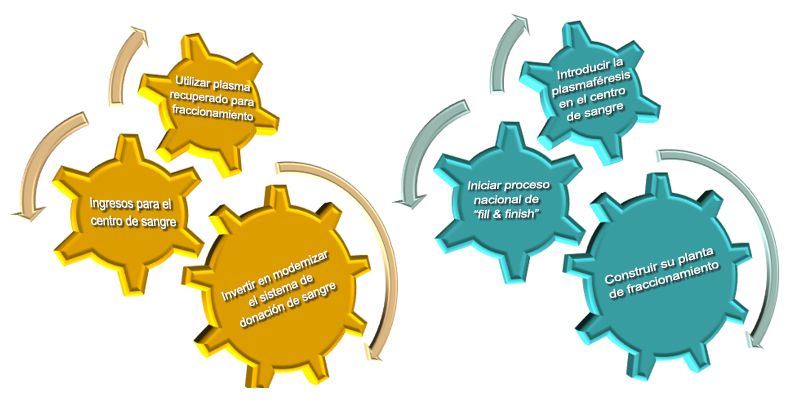
Utilice el ciclo beneficioso.
El primer paso de comenzar a utilizar plasma recuperado puede marcar la diferencia. Usar plasma recuperado para el fraccionamiento crea oportunidades para los centros de sangre.